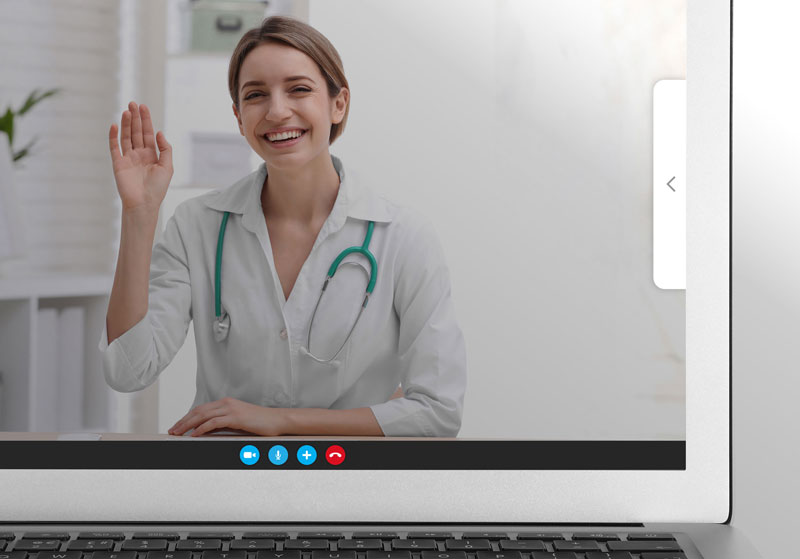
The need for safety during this current pandemic has increased the use of telehealth to provide patient care. Telehealth has been an important part of the healthcare experience, but now, more of society is seeing the advantage of using telehealth with the convenience, flexibility, and safety it provides. Telehealth also brings healthcare to those who are not able to obtain it locally or because of other hurdles that impact an individual patient’s ability to obtain healthcare. As more providers use telehealth, they now see it as a new addition to the healthcare experience that they bring.
When new additions are brought into any experience, it increases the quantity of touchpoints that can provide either positive or negative inputs that impact that experience. Learning more about what these touchpoints are and how to measure and improve them will determine patient and provider success. What used to be just physical touchpoints decades ago has now dramatically shifted to a large combination of both physical and digital touchpoints that impact how a patient perceives their experience. As technology use continues and changes, the quantity of touchpoints will rise. This will put more emphasis on providers to understand how patients take in all these inputs.
Touchpoints to measure in Telehealth
With a patient centered approach, this post will focus on areas that can be measured to improve the patient experience in telehealth. Most patients are now in an environment where uncertainty has increased significantly over this calendar year. Concerns about employment, healthcare coverage, family and individual safety, a way of living, and other changes have impacted patient lives to drive this increased uncertainty. Expectations and perceptions are changing quickly as each person looks to adapt to their new individual and family situations. The importance of having constant feedback and clear communication strategies to understand these recent and future perception changes are vital to improving patient and life experiences. Below you will find three ways to approach measuring these touchpoints to improve the patient experience.
Measuring Senses to Understand Changes in Patient Perception
When a patient first takes on telehealth, it is a new experience to their senses that they have not had the opportunity to learn and make meaning of previously. Providers can perspective take, measure, and then improve the patient experience in telehealth by leveraging the advantages gained over the sensory experiences that have been lost. Since each person has a different history to make meaning of these changes, measuring with feedback is important to improve each individual experience as a provider learns how patients take in these new sensory inputs.
- Sights – What changes do patients see in vision by using telehealth? A patient loses the experience of seeing the whole office, receptionist and staff interactions, the waiting room, and the steps up until the interaction with a physician. Patient vision is now focused on the room they are in, the device in which they are communicating with, and what is on the screen throughout the whole telehealth appointment. Providers can leverage and measure what a patient gains in this new environment. These advantages can include the focused one on one experience with a patient, the autonomy that can be given to a patient to have more control and input into their healthcare experience, and the leveraged use of new technologies to bring a patient and a provider together to improve a patient’s individual health. Areas a provider can measure to improve in sight are:
- Clarity of visuals a patient sees within their appointment
- Distractions at home or in the providers background
- Delays in the visual and/or connection problems that impact the visual experience
- How a patient perceives the appointment visually (Including professionalism, non-verbal cues, visual-emotional connection with the provider)
- Does the visual experience of the telehealth engage the patient to approach and improve their health or does it lead into the direction of disengaging future telehealth appointments and adjustments to their health?
- Sounds – The sounds of a provider’s office change to what is just within the telehealth experience. Providers can leverage this to keep the focus on the information provided to build a stronger bond with their patient. By designing and leading a patient to keep sound distractions away from the appointment, the telehealth appointment can be an effective and productive alternative to office appointments. Within the patient experience in sounds, the following areas can be measured and improved upon:
- The sound quality of the telehealth meeting
- The amount of sound distractions both on the patient and provider side
- The right talking speed, the clarity of the concepts being communicated to the patient, and how a patient understands the verbal communication given by the provider
- Smells and Touches – Moving from the office experience to telehealth, a patient loses positive and negative smells and touches that occur within an office visit. Each provider can go through the losses and gains this change to telehealth does to their individual patients. What can be lost from a patient’s perspective include positive smells of an office that have an association that they are going to be taken care of. Other positive touches lost includes handshakes, a hug, or a provider touching a person to indicate that they are physically measuring to ensure the patient that they are learning the current state of health. These touches lost are important to overcome as they indicate compassion, care, and leadership that the provider will lead the patient to better health.
The senses are vital for a patient to adapt to this new way of health. Learning to understand how a patient is attempting to adapt to this change is important to improve the patient experience. This is even more important for those patients who do not have a strong history of adapting to new technologies.
Using Words to Measure and Improve Telehealth Experiences
A second way to positively impact the patient experience is to start with words that a provider wants the experience to bring to their patients. Using just a word can be a powerful way to start generating ideas and questions along with having a stronger focus on executing a strategy. Below are some one-word suggestions to get started:
- Compassion – How does a patient perceive compassion within a virtual setting?
- Respect – How does a provider respect the time of the patient and them as a whole person? Is privacy and confidentiality kept for the patient?
- Empathy – Does the provider show empathy to the situation that the patient is in and attempts to perspective take on what it would be like to be on the other side? How much energy is focused on the patients’ needs versus the providers or office needs?
- Effectiveness – How effective are the appointments? Are they achieving objectives set with the patient? What results are being seen after a series of appointments?
- Uncertainty – How is the provider addressing patient uncertainty in their lives and this new experience in telehealth? Is the provider addressing billing uncertainty for the patient?
- Engage – Does the patient feel engaged within the appointments to move toward better health and have stronger emotional connections with the provider?
- Communication – Do patients feel confidence in their understanding of what was communicated to them within their appointments? Do providers feel that their instructions are being received correctly by patients?
- Empower – Does the new telehealth experience empower patients to feel better about themselves and the choices they get to make within their health? Does the provider give autonomy in areas to increase patient confidence and improve positive impressions?
- Leadership – Is the provider able to take a lead through telehealth to help the patient not get steered by bad information on the internet and other misinformed sources? Can the provider lead the patient in a positive direction and not be distracted in this new environment?
- Expectations – As positive service is driven by expectations, how are providers understanding and managing expectations to improve the amount of positive experiences a patient has?
Measuring Specific Touchpoints to Improve the Patient Experience
A third way to look at measuring to improve the patient experience in telehealth is to take a patient journey view and measuring important touchpoints along this journey. Measure and improve touchpoints that are important from the patient’s perspective along with touchpoints that providers see as important for their patients’ health and wellbeing. The list below is a starter list but it provides ideas to drive creativity and improve experiences in telehealth.
- Search – How is a provider seen within a search for their services?
- Social Media – How is the provider seen from a patient’s perspective?
- Website – Is the website engaging and informative?
- Setting Appointments – Are they within appropriate range for the patient and do they work with the patient’s schedule? Is the staff friendly and welcoming to patients when they contact?
- Texts and Emails – How are they done and how does a patient perceive their usefulness?
- Patients device in telehealth – Is it working properly? How do sights and sounds work on the device? Is there a good connection? Is there a backup plan if there are problems?
- Telehealth experience – Measure the whole experience as one perception or break it down into parts. Which parts did the patient find useful and where did the appointment go off track?
- Patient Time – Is the provider on time and prepared for the appointment? Did the provider obtain patient questions in advance to make better use of patient time?
- Visuals – Do the visuals within the telehealth make sense to the patient and impact them to make the necessary changes to the provider instructions?
- Interactions on the appointment – Did the provider make it a positive experience for the patient? Did the provider address the needs within the appointment and meet patient expectations? Does the patient understand what is to be expected going forward?
- Prescriptions – What is the plan to make sure the patient gets prescriptions filled, understands the instructions, and stays on track with their plan?
- Billing – Does the patient understand how they are being billed, the insurance aspect, and how they are to pay for the appointments?
- First and Last Impressions – How is the provider managing positive first and last impressions?
- Feedback and post appointment communication – Is the feedback engaging for the patient and how effective is post appointment communications for the patient?
Conclusion
Changes are occurring for patients both in their personal lives and how they are experiencing healthcare. This recent move to a telehealth experience is new for a majority of patients. Individual expectations and perceptions change quickly in times like the present and measuring how a person is perceiving each day is vital to truly making better experiences in a person’s health and in their lives. Providers can take on different ways to creatively measure to better understand how a patient perceives their new experiences. This can be done by measuring perception changes in the senses from an in-office visit to a telehealth experience.
It can also be done by starting with words that represent what a provider wants to bring to a patient experience and then expand that out. Lastly, it can be done by listing and measuring important touchpoints of a patients journey in their healthcare experience. With technology and world changes occurring faster, providers can be leaders by having a mechanism of feedback and communication that is patient and human focused. This allows the provider to be on top of changes and being proactive versus falling behind and reacting to the changes that occur.
About SmileyAnswers
SmileyAnswers provides real-time actionable insight by utilizing the HappyOrNot® Reporting Solution. The HappyOrNot® Reporting Solution is trusted by over 600 healthcare systems and has collected over 1 billion feedbacks from around the world. By collecting real-time feedback, healthcare providers are able to find hidden pain points quicker to make more positive changes in the patient experience.
As a way to help healthcare providers adapt and thrive in this new environment, SmileyAnswers introduces two new Smiley’s that “GoTouchless”. The Smiley Link is used to collect real-time feedback with a QR code that is attached to a Smiley Touch or a Smiley Terminal. The patient has the option to give feedback right at the terminal or through using the QR code. The second addition to the Smiley family is the Smiley Digital. This effective new option increases the amount of ways that providers can obtain real-time insight through their digital and physical touchpoints.